Malaria
Created | Updated Dec 13, 2011
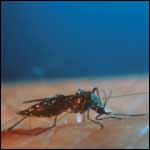
'Name a dangerous creature'
Ask a European child this question and the answer you get will probably feature claws, teeth, whiskers and either stripes or a shaggy mane. Ask an African child, and the answer might well be surprising, since the deadliness of the creature in question may well seem out of all proportion to its size. This animal, the mosquito, is the world's worst spreader of blood-borne diseases. The most undoubtedly pernicious of these diseases originates from transmission of, and subsequent infection by, a protozoan parasite, Plasmodium that lurks in the salivary glands of the mosquito.
Plasmodium is the sole cause of malaria, a disease, which by latest estimates will bring misery to between four and five hundred million people this year. Of these, it will kill about a million1, mostly children under five. By the time you have finished this Entry, between 20 and 30 children will have died from malaria, and that's just in Africa2 Unlike many contagious diseases, malaria shows no signs of dying out. If anything, the disease is on the increase as the virulent parasite develops resistance to an expanding range of drugs.
Compared with the (successful) wars waged against smallpox and now polio, the skirmishes with malaria are being fought on a large number of fronts with all-too-few resources and, unsurprisingly, few significant and lasting victories. Despite the lack of prominence given to it compared to, say, AIDS, malaria is an extensive and growing threat and its total eradication is viewed as near impossible. It is nevertheless both treatable and preventable.
Know Thine Enemy - the Malarial Parasite
All malaria is caused ultimately by infection with Plasmodium . Plasmodium is a protozoan: a singled-celled organism with a well-defined nucleus (unlike a bacterium). There are four species of Plasmodium that cause human malaria: P. falciparum is the most dangerous. Thanks to the thousand fold increase in the number of genes that that it carries over the AIDS virus, Plasmodium exhibits a lifecycle of Byzantine complexity. The main purpose of this bizarrely complex cycle seems to be both to hoodwink the human immune system into letting it get away with cellular hooliganism on a huge scale, and to combine the evolutionary advantages of both sexual and asexual reproduction.
This cycle can be said to start with a single, nocturnal mosquito bite, as far as the unfortunate victim is concerned. The salivary glands of the mosquito inject anticoagulants into the bloodstream to prevent their meal from clotting. Hitching a ride on these fluids is one form of Plasmodium: sporozoites. These live in the salivary glands and those that manage to make it into the bloodstream make their way to the liver. Only half a dozen of these tiny parasites may be injected at this point.
Once in the liver, the sporozoites infect a liver cell and become a cyst. Cocooned away from the scrutiny of the immune system, they perform the first of the change of identities that characterise this disease, and become tens of thousands of malaria's shock troops: merozoites. This process takes about ten days – just short enough for the immune system not to become aware – and the victim will have probably only an itchy swelling to show for it at this point.
The situation changes dramatically when the merozoites are released into the bloodstream. They make straight for, and infect, red blood cells and immediately start to devour the oxygen-carrying haemoglobin protein. Over two to three days, the merozoites multiply up to 24 times. After they have eaten everything they can find, they burst from the red blood cell and seek out others to infect. As this sub-cycle of consumption and division repeats itself, the victim is struck by a wracking fever that comes on when the merozoites burst loose. As if this were not bad enough, the chronically afflicted also suffer anaemia and lethargy through lack of blood oxygen: in a few hours the merozoites can eat a quarter of a pound of oxygen-carrying-haemoglobin.
At this time, the body's immune system is beginning to sit up and take notice that something is very seriously wrong. Normally the services of the spleen would then be called into play to mop-up and destroy infected blood cells, and the unchanging nature of the parasite during this phase should prove an Achilles' heel, allowing the immune system to get to know its enemy long enough to mount an effective response.
Plasmodium has another microbiological countermeasure up its sleeve, needless to say. Not only do the merozoites set about cleaning out the contents of their new dwelling places, but they set about the infrastructure as well. They make the membrane of the host cell sticky, so that they lodge in small capillaries and never get to the spleen. The damaged cell drops anchor and its cargo breeds undisturbed in the quiet backwaters of the circulatory system, never having to brave the immunological maelstrom of the spleen.
After fever, a malaria sufferer may have another gauntlet to run: cerebral malaria. The logjam of damaged red blood cells in the capillary system, overrun by piratical merozoites, becomes particularly acute in the brain. The amount of oxygen reaching brain cells can drop off, so much so that the victim lapses into a coma. At this point, death is highly likely in an untreated patient.
After infecting red blood cells, some merozoites don't divide but turn themselves into either sperm or eggs, referred to as gametocytes. They then sit tight, waiting for the next mosquito to bite. When they get into the mosquito's gut the gametocytes change into yet another form and set about finding other changed gametocytes (possibly from other strains of malaria) to fuse with to form fertilised eggs, or zygotes. These then change yet again into ookinetes that move into the gut wall, form cysts, and divide into thousands of sporozoites. Once these are released from their cyst, they make their way to the mosquito's salivary glands, ready to infect another person.
Combatting the Disease
If you have lost track by this point of the number of disguises that the parasite has adopted, it's hardly surprising that the non-sentient human immune system has an even harder job keeping up3. This of course is the point behind the parasite's lifecycle: it generally doesn't stay in one form long enough to be recognised as an enemy, and when it does it skulks well away from possible danger. Its chameleon-like nature is one of the features of Plasmodium that make it such a troublesome adversary.
The parasite's virulence, on the other hand, arises from the fact that the mosquito vector transmits it indirectly. The human host can be bed-ridden or at death's door, and still infect tens or hundreds of other people, so it's not in the parasite's interest to preserve its host for as long as possible, but to exploit the host as much as it can before the immune system belatedly kicks in. Eradicating Plasmodium entails developing a degree of cunning better than that shown by the parasite itself.
Shoot the Messenger
The lifecycle of the parasite is both its greatest strength and weakness. Each stage in the parasite's development offers us an opportunity to attack it with a new tactic. Unfortunately, the most obvious points of attack have ended up being the least productive. Control and containment have therefore become the watchwords in the campaign against it.
Initially, attacks concentrated upon the vector: the Anopheles mosquito. During the 1940s there was a concerted effort to rid the world of malaria by eradicating the mosquito. Predictably4, indiscriminate use of the insecticide DDT meant that mosquitoes themselves became resistant to the insecticide.
Despite this development, DDT still remains one of the most effective weapons against malaria when used in a contained and responsible fashion. Preventing mosquitoes from getting at their evening meals is a particularly effective way of limiting the effects of the disease. Sending children to bed early and using bed nets treated with the chemical can cut infant mortality by 30%5. Also, even after their meal there is scope to prevent the further spread of the disease. Mosquitoes tend to rest on walls when they are digesting blood after a meal, and treating these walls with DDT kills them.
Simple expedients such as putting glass in windows can prevent mosquitoes from biting their victims: even Britain used to be a stronghold of malaria during Roman times, but since the population moved out of the countryside into cities and towns to live in substantial houses, the endemic has disappeared.
One of the most intriguing yet remote prospects for control of malaria transmission via mosquitoes is to somehow prevent the mosquito itself from transmitting the disease. This would entail genetically engineering mosquitoes to resist infection by the parasite. Getting the altered genes to spread throughout the mosquito population is a bigger problem.
Vaccination
Trying to boost the immune system's response to Plasmodium through vaccination has, up to now, been spectacularly unsuccessful: the ever-spreading domain of the parasite is a testament to this failure. When the human immune system responds to an invading threat it does so by recognising antigens (proteins) on the invader's cell membrane and then loosing the correct antibodies against them. The malarial parasite exhibits different antigens on its surface at different stages in its lifecycle, whereas viruses and bacteria generally don't. Even more dismayingly, the parasite attacks the body in waves, each wave having different antigen proteins on its cell membrane. Vaccination against malaria is therefore like trying to forearm against a target that constantly changes its armour.
The only current effective way of vaccinating against malaria is to allow oneself to be bitten at least 1,000 times by mosquitoes irradiated with gamma rays: hardly an option in tropical Africa. This treatment damages the sporozoites so that they cannot hide away in the liver. The immune system then has chance to recognise them and develop antibodies: the target is stopped dead in its tracks long enough for the immune system to take effective aim.
Ironically, one of the organisations most active in the quest for an effective malarial vaccine is better known for taking lives than preserving them. The US Navy has many troops overseas, and these are at particular risk from infection: malaria accounted for more American casualties in Vietnam than bullets. Unlike most approaches so far, the Navy's approach is to attempt to provoke resistance against the parasite at every stage of its lifecycle by using fragments of the parasite's DNA to make malarial proteins. This approach is promising, but still under development.
The major drawback to vaccination is that it is unlikely to be 100% effective in preventing infection, leading to the evolution of even more resilient and dangerous strains of the disease. The 'nightmare scenario' envisages a few vaccinated individuals carrying, rather than suffering from hyper-virulent malaria, and acting as reservoirs for infection of the less well protected. Vaccination is an all-or-nothing option and the current state of progress makes the use of a partially effective vaccine downright foolhardy.
Drug Treatment
Drugs can be administered in two ways: as preventatives or curatives. The first effective antimalarial drug was quinine, prepared from the bark of the cinchona tree. Most strains of falciparum are now resistant to quinine, and the modern alternative, chloroquine is becoming less effective. Mefloquine, another modern antimalarial, is deemed too expensive for widespread and persistent use among the people most likely to suffer.
The current 'wonder drug' in the treatment of malaria is qinghaosu (artemisinin), a Chinese herbal remedy known for 2,000 years (in China, at least). Qinghaosu is obtained from a species of artemisia (wormwood), its active ingredient being a highly strained molecule, rich in oxygen. Iron catalyses the explosive and energetic breakdown of this molecule so merozoites, rich in iron, are destroyed when they come into contact with the drug. This process happens so fast that the parasite may not have time to mount an effective defence against the drug, even if it has access to one. The hope is that qinghaosu will continue to be a reliable and effective treatment for infected patients indefinitely.
One new drug currently undergoing trials, G25, attacks the merozoites by preventing them from making a protective membrane within the red blood cell. G25 has been shown to kill all merozoites within two days, and remarkably the parasite did not develop resistance to the drug. Unfortunately, G25 needs to be injected and so requires administration by trained staff. Its developers are now looking to develop an oral form of the drug that could be distributed and taken easily.
Unlike vaccination, drug treatment does not need to eradicate, rather merely control. During its asexual reproductive phases, Plasmodium is as prone to mutation, and therefore adaptation, as any bacterium. Attacks mounted by the immune system or drugs in these phases can serve to exert evolutionary pressure upon the parasite to its ultimate benefit despite the short-term harm caused to it. However, combinations of drugs can serve to prevent resistant strains from arising through a 'double-whammy' effect: the parasite would have to develop double resistance through one mutation in order to be able to survive. Artemisinin and chloroquine are two drugs that are cheap and effective when given in combination.
Future Prospects
Ultimately, malaria is treatable, far more so than TB or AIDS. New approaches such as novel vaccines or drugs are likely to be needed only in areas where malaria is rampant. In other areas, the disease could be successfully controlled by the simple measure of combination drug therapies, handing out bed nets, putting glass in windows and even throwing away old tyres so that larvae cannot breed in them.
It is probably not because we lack the weapons, but the will, that this disease continues to be a scourge of those whose only crimes are to be young, poor and living in a developing country. To state that 'Plasmodium is responsible for the huge malarial death toll' is akin to saying that 'everyone dies from heart failure': superficially correct, but glib and intellectually dishonest. There are many points in the progress of the disease during which malaria could be routed, and its continued and profound impact is more an issue of politics and money than science and health practice.
It's nevertheless a battle worth fighting, since by conquering malaria, a virtuous circle is established, of increased prosperity leading to better health6. Malaria is to a large degree preventable, treatable and curable in a cost-effective manner: a single bout in an African adult is equivalent to ten lost workdays, whereas the drugs to treat it vary from cents to a few dollars. It is therefore a disease characteristic of poverty: poverty in prevention, of effective treatment and of determination of prosperous countries in failing to square up to this ancient scourge on behalf of the less wealthy. There are good reasons for failing to eradicate this disease so far, but no good excuses for the scant progress made to date in reducing its capacity for causing suffering and death.
Finally, there is one overriding reason why the defeat of malaria should be made a global priority: it is on the march again. Much of its recent spread is attributable to it retaking lost ground as Plasmodium develops resistance to drugs. More alarmingly, as the global climate warms up, malaria will find it easier to establish a foothold in new breeding grounds. It is in the interests of the developed world to win a decisive battle against malaria on its own territory, before it finds itself having to fight one in its own backyard.

